Multi-component strategies for cholesterol control beyond adherence
July 14, 2025Pharmacy researchers at the National University of Singapore (NUS) have demonstrated that multi-component interventions are required to improve the regular intake of cholesterol-lowering medications.
Despite the established effectiveness of lipid-lowering medications (LLMs) in reducing cholesterol for the prevention of heart disease and stroke, many patients either do not take their medication regularly or discontinue it prematurely. Prior studies have explored various interventions aimed at improving LLM-taking behaviours, also known as medication adherence, and have demonstrated some degree of effectiveness. However, details on how adherence was measured and how these interventions impacted cholesterol levels over time were often lacking.
To address this, a research team led by Associate Professor Doreen TAN Su-Yin from the Department of Pharmacy and Pharmaceutical Sciences at NUS systematically reviewed published information in scientific journals on interventions designed to improve adherence to LLMs for the prevention of heart disease and stroke, and evaluated their effectiveness in managing cholesterol levels. Their study aimed to identify the most effective and sustainable intervention strategies as well as to clarify the relationship between improved adherence and longer term cholesterol control. This work was performed in collaboration with clinical psychologists from the Lee Kong Chian School of Medicine at Nanyang Technological University.
Their findings were published in the journal eClinicalMedicine.
The research team screened more than 21,000 abstracts published between January 2016 and October 2024. Of these, 35 studies were shortlisted for the systematic review, and 15 were analysed in detail. The review found that the most effective interventions involved complex behavioural modifications that included understanding and addressing a patient’s motivations in combination with incentivisation. Other promising strategies included frequent follow-up by healthcare professionals and patient education on their medical conditions and medications. However, these effects generally did not last beyond a six-month period, nor did they lead to meaningful improvements in blood cholesterol levels.
The team’s findings suggest that single-mode interventions are likely to be limited in their effectiveness in improving the complex problem of poor adherence to LLMs and blood cholesterol lowering. This evidence supports the implementation of multi-component strategies consistent with the World Health Organisation’s (WHO) five-dimensions of medication adherence framework, particularly the behavioural, educational and administrative dimensions. Beyond patient-related factors, the study team recommended greater emphasis on condition-related and healthcare team factors, such as clinician engagement in optimising therapy and achieving blood cholesterol targets. A shift toward more comprehensive, system-level strategies is needed to yield sustained improvements in adherence and meaningful cholesterol-lowering effects.
The team found that most interventions aimed at improving medication adherence targeted only one aspect of the WHO’s five-dimension framework, resulting in short-term benefits that rarely extended beyond six months. They recommended adopting multi-faceted strategies that address multiple dimensions, including active involvement of the healthcare team to achieve lasting improvements. The review also underscored the importance of using both objective and subjective measures to assess adherence. Indirect methods such as pill counts, prescription refill rates and electronic monitoring were the most commonly used due to their objectivity, while subjective tools like beliefs and values questionnaires provided valuable insights into barriers to adherence. Despite modest improvements in adherence, there were no significant changes in cholesterol levels, highlighting the need for more comprehensive interventions that also include healthcare and system-level factors.
Associate Professor Tan said, “If you wish to go fast, go alone. If you wish to go far, go together. Our study highlights both the value and limitations of current approaches, and calls for more holistic, long-lasting solutions.”
Future interventions to improve adherence to LLMs should address multiple dimensions of adherence to foster sustained, long-term results. For achieving greater impact on patient outcomes, future studies should also address clinician prescribing practices and incorporate non-pharmacological strategies, rather than focusing solely on adherence.
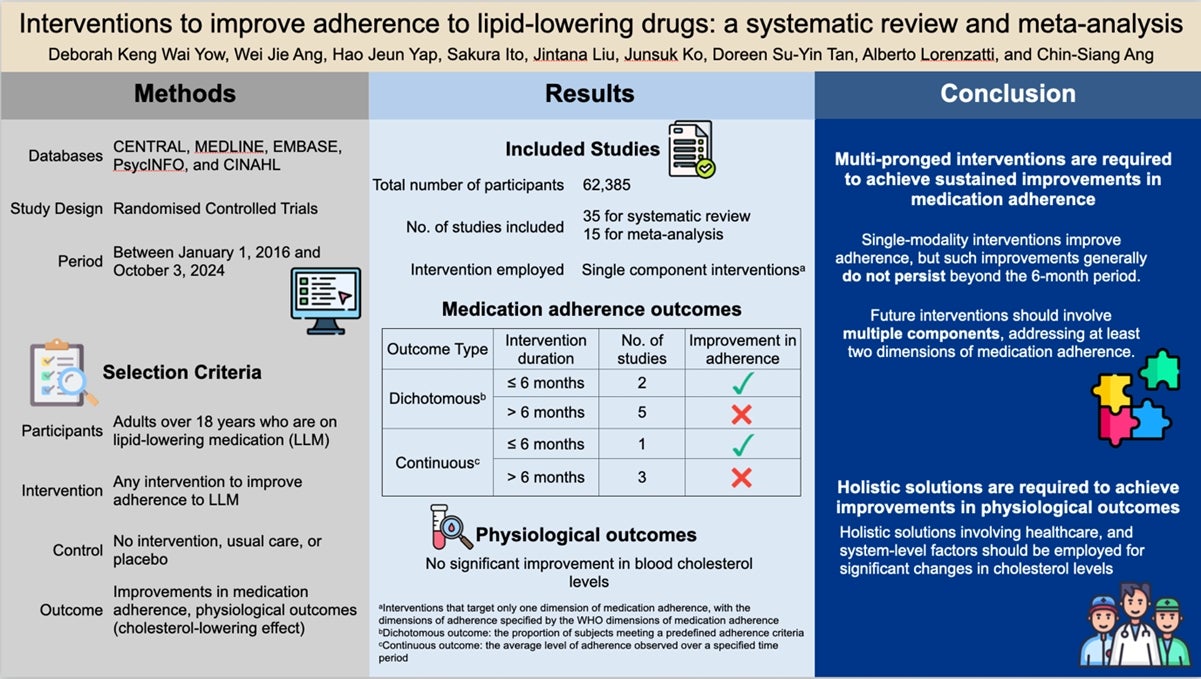
A systematic review showing that single-component interventions improve short-term adherence to lipid-lowering drugs but fail to sustain effects beyond 6 months, highlighting the need for multi-pronged and holistic strategies for long-term adherence and cholesterol reduction.
Reference
[1] “Adherence to Long-term Therapies: Evidence for Action”, World Health Organization Published: 2003.
[2] DKW Yow; WJ Anga; HJ Yap; S Itob; J Liu; J Ko; DSY Tan*; A Lorenzatti; CS Ang, “Interventions to improve adherence to lipid-lowering drugs: a systematic review and meta-analysis” eClinicalMedicine, Volume: 84 103270 DOI: 10.1016/j.eclinm.2025.103270 Published: 2025.


